Anti-Vascular Endothelial Growth Factor Agents for Diabetic Macular Oedema
Diabetes can make the blood vessels at the back of the eye leak. This can lead to waterlogging/swelling at the back of the eye called Oedema.
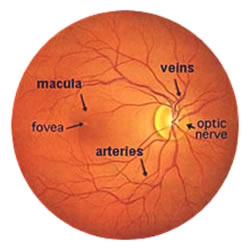
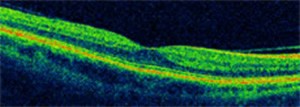
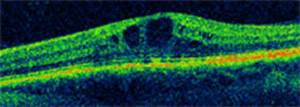
The most important part of the retina for eyesight is called the Macula and hence swelling of this part is called Macular Oedema. When this Oedema is at the centre of the retina it can reduce eyesight. Oedema is normally assessed using an Optical Coherence Tomography scanner.
The mainstay of treatment for Diabetic Macular Oedema (DMO) is retinal laser. This was shown 25 years ago in the Early Treatment of Diabetic Retinopathy Study (ETDRS) to be effective at reducing the chance of eyesight deteriorating when Oedema threatens to spread into the centre of the macula (the fovea).
Conventional laser is not always effective at preventing deterioration of eyesight or improving eyesight when the Oedema has already reached the centre however. Because of this doctors have looked for other treatments to treat centre involving DMO.
The first treatment that was tried was intraviteal injection of steroid. Although this initially seemed to be quite effective, as time went by it was shown that it was no better than laser.
One of the chemicals that is involved in making the blood vessels leak is Vascular Endothelial Growth Factor. There are drugs which have been used to block this chemical in Age Related Macular Degeneration, Avastin and Lucentis, which have now been shown to be of benefit in centre involving DMO.
There are several studies comparing Lucentis (READ 2, RESTORE, RESOLVE and DRCR.net), Eylea (VIVID and VISTA) or Avastin (BOLT and DRCR.net) with laser.
There is one large-scale randomized trial comparing Lucentis, Eylea and Avastin for diabetic retinopathy, the DRCR.net protocol T study.
In general the studies have shown that if you have an Anti-VEGF course of injections rather than laser, your eyesight is likely to be 1 and ½ to 2 lines of vision better after 2 years than with laser on its own.
The DRCR.net study showed that for patients with good vision, there was little difference between Lucentis, Eylea and Avastin. If you have worse vision however, Eylea appeared to be slightly better than Lucentis and Avastin.
“I have no words to adequately convey my thanks for the cataract operation that you performed on me. Life changing does not come close to explaining the difference in my vision and I will be forever grateful.” Mrs B, Chippenham
How many injections will I require?
The studies so far have all been different and it is not known how many injections to give and for how long. My personal recommendation is to have a loading dose of 5 to 6 injections and then review monthly thereafter to see if any more injections are needed.
Research studies have suggested an average of 14 to 16 injections over 2 years.
Should I have laser as well?
It is not clear yet whether laser gives additional benefit when given together with intravitreal injections; some studies have suggested that there might be a small additional benefit over the long term but others have not shown any additional benefit.
Intravitreal steroid injection
There are 2 steroid injections that are also used for Diabetic Macular Oedema; Ozurdex and Iluvien.
Ozurdex lasts 4 to 6 months and is given as an alternative to Anti-Vascular Endothelial Growth Factor Agents. Research has suggested that it is not quite as effective, but you need fewer injections.
Iluvien lasts for 3 years and is given when other treatments don’t work or have stopped working, and when the Oedema has been present for at least a year and a half.
The main additional risk factors for these injections are that they can cause the pressure inside the eye to rise and that they cause cataracts. The pressure can usually be controlled with drops and these agents are not normally given to someone who hasn’t yet had cataract surgery.
